What We offer
Discover Ways To Tackle Mental Health Crisis.
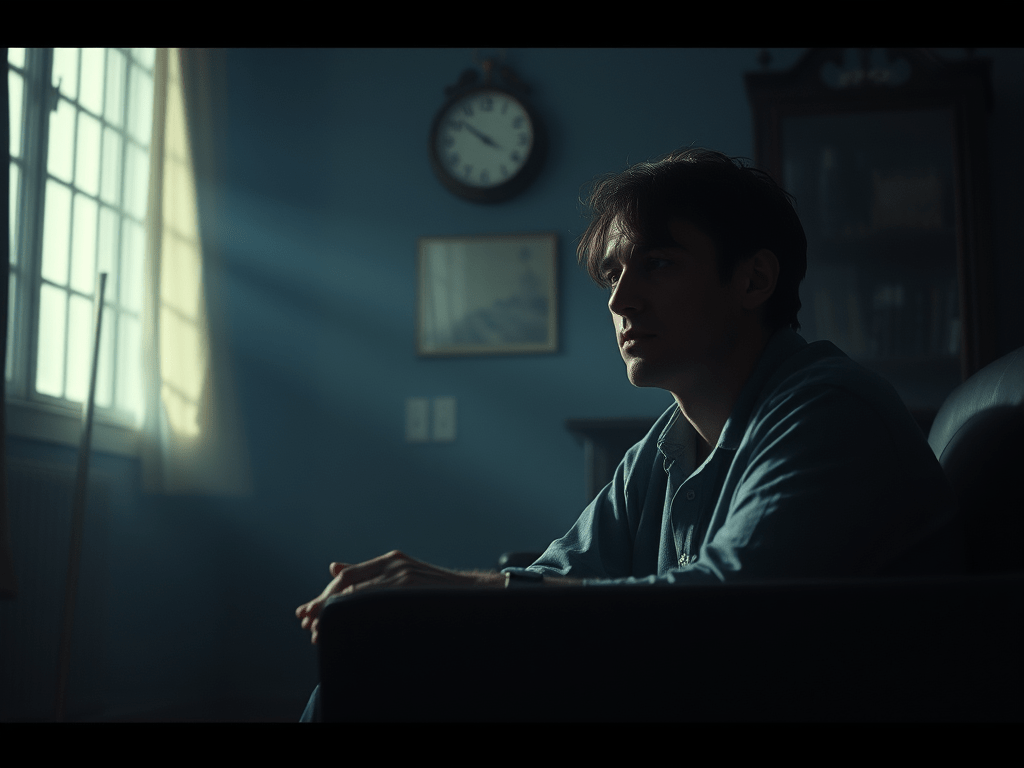
Mental health recovery is a deeply personal and often painful journey — and it’s okay to experience setbacks along the way. Even after making progress, it’s possible to relapse or find yourself in crisis again. What matters is recognising the early signs, having a plan in place, and holding onto the hope that things can improve. Recovery isn’t about perfection — it’s about accepting your challenges, showing up for yourself, and making the most of each step forward, no matter how small

What is Crisis?
Many great thinkers of the past have spoken about emotional struggles, mental confusion, and personal turmoil. Socrates and Plato believed that when we feel lost or uncertain, it may be a signal to pause and reflect on our lives. Such moments, though painful, can also serve as powerful turning points—opportunities for growth and deeper self-understanding.
While modern psychology and psychiatry offer clinical terms to describe mental health crises, philosophy offers a more human-cent red perspective. It views crisis not merely as a disorder, but as a rupture—an opening for transformation. From this lens, a crisis is not just something to survive, but a moment that can lead to clarity, insight, and renewal.
Importantly, crisis is defined by each person’s unique experience. What feels overwhelming to one individual might not affect another in the same way. That’s why it’s important to acknowledge and accept your own struggles without comparison or judgment. By recognizing your emotional state and responding with empathy—through reflection, seeking support, or making meaningful change—you begin to open the path toward healing and recovery.

Understanding Mental Health and Relapse
Understanding your mental health condition is a gradual, evolving process. Symptoms and experiences can shift over time, which is why regular self-reflection — such as keeping a mental health journal — can be especially helpful. Developing insight into your personal triggers, patterns, and treatment options empowers you to make informed decisions about your care. You have the right to choose the approach that best suits your needs and to adapt it as those needs change. However, any changes to therapy or medication should always be discussed with a qualified clinician, to ensure they are made safely and effectively.

Benefits of Engaging with Mental Health Services
Connecting with mental health services provides expert support, personalised care, and access to tools that can help you stabilise, recover, and thrive.

Advance Statements
An advance statement is a written document that outlines your preferences for treatment and care in the event of a future mental health crisis, especially if you’re unable to express your wishes at the time. It helps ensure your voice is heard by professionals, guiding decisions about medication, hospital care, and support strategies based on what works best for you. Creating one in advance can reduce stress during crises, support personalised care, and involve trusted people in your recovery plan.
Learn and Grow
What to expect After a Mental Health Crisis Assessment
Experiencing a mental health crisis can be overwhelming and confusing. If you’ve recently undergone a mental health crisis assessment, you might be wondering what happens next and how the support system will help you move forward. Understanding the process after a crisis assessment can ease anxiety and empower you to take charge of your recovery.
In this article, we explain what typically happens after a mental health crisis assessment, including possible hospital admission, community support options, and follow-up care.
What Is a Mental Health Crisis Assessment?
A mental health crisis assessment is a comprehensive evaluation conducted by trained professionals to understand your current mental health state, assess any risks to yourself or others, and determine the best course of action. These assessments can be carried out by crisis teams in the community or liaison psychiatry teams in hospital settings like Accident & Emergency (A&E).
The goal is to quickly identify the severity of the crisis, your needs, and the support available to keep you safe.
Possible Outcomes After a Crisis Assessment
1. Hospital Admission
In some cases, hospital admission may be necessary to provide intensive care and ensure safety. There are two types of hospital admission:
- Voluntary (Informal) Admission: You agree to be admitted to the hospital and participate in treatment voluntarily.
- Compulsory Admission Under the Mental Health Act: If you are assessed as lacking capacity to make treatment decisions or are at significant risk of harm to yourself or others, you may be admitted under legal powers to protect your safety.
Hospital stays provide 24/7 monitoring, medication management, and access to multidisciplinary mental health teams.
2. Crisis Resolution and Home Treatment Team (CRHTT)
If hospital admission is not required, you may be referred to a Crisis Resolution and Home Treatment Team. This team offers intensive support at home as an alternative to hospital.
The CRHTT will ensure you can stay safe in your community, either independently or with the help of family or carers. Services typically include:
- Daily or twice-daily visits from mental health professionals
- Medication management and monitoring
- Assistance with coping strategies and crisis planning
- Support from doctors, nurses, occupational therapists, and others
This approach helps you remain in your familiar environment while receiving expert care.
3. Referral to Community Mental Health Services
If your immediate crisis resolves but you need ongoing support, the crisis team or your GP may refer you to community-based mental health services such as:
- Community Mental Health Teams (CMHT): Provide ongoing assessment, treatment, and support for people with long-term mental health conditions.
- Talking Therapies: Including cognitive behavioural therapy (CBT) or counselling.
- Substance Misuse Services: If drug or alcohol use contributes to your mental health.
- Peer Support Groups and Social Prescribing: To connect with others and access community resources.
These services help you build resilience and manage your mental health over time.
4. Discharge Back to Your GP
If your needs can be managed within primary care, you may be discharged back to your GP with advice and treatment plans to continue your recovery.
If you feel your concerns have not been fully addressed or you require additional specialist support, don’t hesitate to discuss this with your GP. They can make direct referrals to appropriate mental health services on your behalf.
How to Prepare for Aftercare Following a Crisis Assessment
- Ask Questions: Make sure you understand your treatment plan and who will be involved.
- Engage Your Support Network: Involve trusted family members or friends to support you.
- Know Your Emergency Contacts: Keep crisis helpline numbers and local services handy.
- Attend Follow-Up Appointments: Regular contact with healthcare providers is crucial.
- Practice Self-Care: Use coping strategies and attend therapy sessions as recommended.

Traffic Light System
Green: Low Risk – Stable, but In Need of Extra Hand
You are generally stable and managing well with daily activities. However, you still need some extra hand in areas of life that may feel overwhelming.
Signs You’re in the Green Zone:
- You are calm and composed.
- You are generally maintaining a healthy social connections.
- You are taking care of your physical health and maintaining your self-care
- You have a positive attitude and are optimistic about the future
- You can think clearly and logically. However,
- You need help with practical matters like housing, finances, claiming benefits, legal battle or vocational support.
What You Can Do:
- Contact family members or friends for support
- Contact your GP or care coordinator, if you have one
- If you are under long-term mental health services, contact your team.
- Reach out to Citizen Advise Bureau for general advice.
- Visit a Safe Space or community centre for non-urgent support.
- Call MIND for mental health resources and information.
Amber Zone: Moderate Risk:
Right now, things might feel unmanageable, but you’re not alone — and you’re not in crisis just yet. This is your opportunity to take some early, empowering steps to protect your mental health and prevent escalation.
What You Might Be Noticing:
- Feeling like you’re on the edge of a relapse or mentally declining.
- Experiencing more worry, hopelessness, or irritability.
- Having mood swings — feeling very low at times, then unusually high or energetic.
- Struggling with concentration, thinking clearly, or daily functioning.
- Eating and sleeping are out of balance, and it’s affecting your energy or mood.
- You’re withdrawing socially or feeling suspicious or unmotivated.
- Your medications don’t seem to help, or you’re considering changing them on your own.
What You Can Do
- Talk to someone you trust
Let a friend, family member, or someone you’re comfortable with know how you’re feeling. - Visit a Safe Space or take quiet time
Find somewhere peaceful where you can breathe, reflect, and feel safe. Many communities have local Safe Spaces designed for this exact need. - Join the 1in4 Forum – the UK’s largest online mental health community
You can connect with others who are going through similar struggles. - Call the Samaritans – 24/7 listening support
They’re here for you, no matter how big or small your struggles feel.- UK Helpline: 08457 90 90 90
- ROI Helpline: 01 850 60 90 90
- www.samaritans.org.uk
- Call SANE – emotional support and mental health guidance
Ideal when you’re overwhelmed, stuck, or just need someone to talk to.- Helpline: 0845 767 8000
- www.sane.org.uk
- Contact SPA – Single Point of Access
SPA services are different in each local area, and they are your gateway to NHS mental health support.- To find the right SPA for you, search your local NHS Trust website or call your GP for the correct number.
- SPA teams can help assess your current mental health needs and connect you with the right service, whether it’s urgent or ongoing care.
- Talk to your GP
Let your GP know what’s going on — especially if your medication isn’t working or you’re feeling worse. They can help make clinical decisions with you. - Speak with your mental health team
If you’re already under specialist care, check in with them. They can adjust your care plan and offer extra support. - Contact your care coordinator
- Let them know you’re struggling. They can help you coordinate your next steps, book appointments, or check in more frequently
Red: High Risk – Immediate Mental Health Crisis
This is a severe and urgent situation. You or someone else may be in immediate danger. Taking urgent action is essential to stay safe.
Signs You’re in the Red Zone:
- You are in distress, and you don’t know what to do next.
- You may be thinking about harming yourself or ending your life.
- You may have started to self-harm.
- You feel extremely paranoid, believing someone wants to harm you.
- You may become verbally or physically aggressive.
- You’re experiencing hallucinations, delusions, or disorganised thoughts.
- You feel vulnerable, and without help, you may experience serious harm.
- Your speech is confused, and your thoughts aren’t making sense.
- Whatever you try doesn’t seem to help—you feel stuck or hopeless.
What You can do:
- Go directly to the nearest A&E (Accident & Emergency) if you can.
- Ask a friend or family member to take you to A&E.
- Contact your local Crisis Team or Rapid Response Mental Health Team.
- Call NHS 111 or your local SPA (Single Point of Access) service.
- Call 999 if you or someone else is in immediate danger.
- Call the police if there is a threat of harm to yourself or others.
Crisis Contact Numbers (UK)
Emergency Services: 999
NHS 111: Non-emergency medical support
Samaritans (24/7): 116 123
Crisis Text Line: Text SHOUT to 85258
Reflections
Online Resources
Take a Action
Green Zone
Mind: Mental health information, wellbeing tips, and legal rights
Citizens Advice: Help with benefits, housing, and legal or financial issues
Rethink Mental Illness: Support for managing long-term mental illness and finding advocacy
Every Mind Matters – NHS: Build a mental wellbeing action plan
1in4 Forum: Peer support and discussion in a safe online community
Amber Zone
SHOUT Text Line: Text SHOUT to 85258 for 24/7 crisis support
Samaritans: Call 116 123 for confidential listening and support
SANEline: Call 0300 304 7000 for evening mental health support
1in4 Forum: Connect with people who understand what you’re going through
Togetherall (Big White Wall): Anonymous online support community with clinical moderation
Red Zone
Emergency Services: Call 999 if in immediate danger
NHS 111: Call 111 for urgent but non-emergency mental health help
Samaritans (24/7): Call 116 123
SHOUT Text Line: Text SHOUT to 85258 for immediate crisis support
Go to A&E: Visit your local A&E if you’re in urgent mental health crisis
Contact your local Crisis Team / SPA (Single Point of Access): Found via your local NHS Trust or GP