A mental health crisis doesn’t always look like chaos. Sometimes it looks like success. Sometimes it sounds convincing. Sometimes it hides behind intelligence, generosity, or confidence.
Bipolar Affective Disorder (BPAD) is one of the conditions most often misunderstood in crisis; not because it is rare, but because its symptoms are frequently misread, rewarded, or dismissed until real harm occurs.
Why BPAD Crises Are Missed Today
In modern culture, behaviours linked to BPAD are often praised:
- sleeping little while staying productive,
- bold decision-making,
- intense confidence,
- generosity without limits.
At the same time, deep exhaustion, withdrawal, or hopelessness are dismissed as stress or weakness.
This means that a BPAD crisis may go unrecognized until:
- all your money is gone,
- your relationship is strained,
- you are facing legal trouble or encounter risks to your safety
- or suicidal thoughts emerge.
The Two Main Crisis Patterns in BPAD
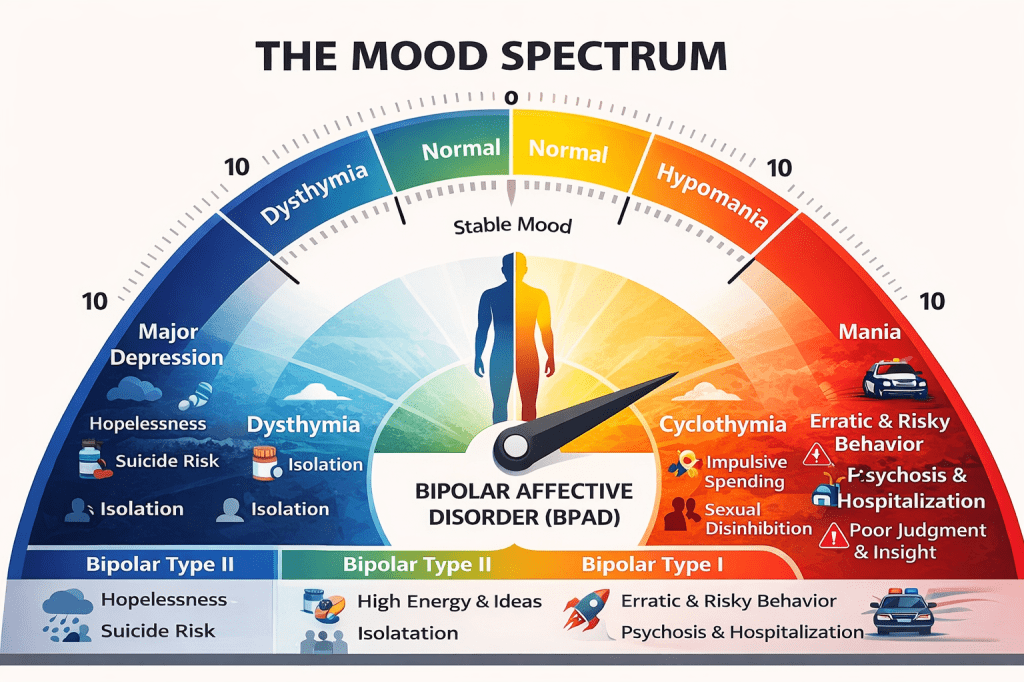
Depressive Crisis (Low Phase)
This crisis is often quiet but extremely dangerous.
Common signs
- Withdrawal from people and responsibilities
- Profound fatigue or slowed thinking
- Loss of hope or meaning
- Intense guilt or worthlessness
- Changes in sleep and appetite
- Thoughts of death or suicide
Why this is a crisis
- Suicide risk is high
- The person may appear calm while suffering deeply
- Help is often delayed because distress is internal
Manic or Hypomanic Crisis (High Phase)
This crisis is often misinterpreted as confidence or drive.
Common signs
- Little or no sleep without tiredness
- Racing thoughts and nonstop speech
- Unrealistic plans or grand ideas
- Irritability when questioned
Specific crisis behaviours
- Sexual disinhibition or unsafe behaviour
- Overspending or sudden debt
- Giving money to strangers or unrealistic causes
- Reckless driving or impulsive travel
- Sudden life-changing decisions
Why this is a crisis
- Judgment is impaired
- Insight is often lost
Financial, legal, and physical risks escalate quickly
Mixed Episodes: A High-Risk Crisis State

Insight, High Achievement, and Hidden Crisis
Insight — the ability to recognize illness — often changes during BPAD episodes.
- In depression: insight may be present but distorted by hopelessness
- In mania: insight is often absent
For high-achieving or high-functioning individuals, crisis is even harder to recognize:
- hypomania may coincide with success,
- warning signs are praised,
- help feels like a threat to identity.
This does not protect against crisis — it delays recognition.
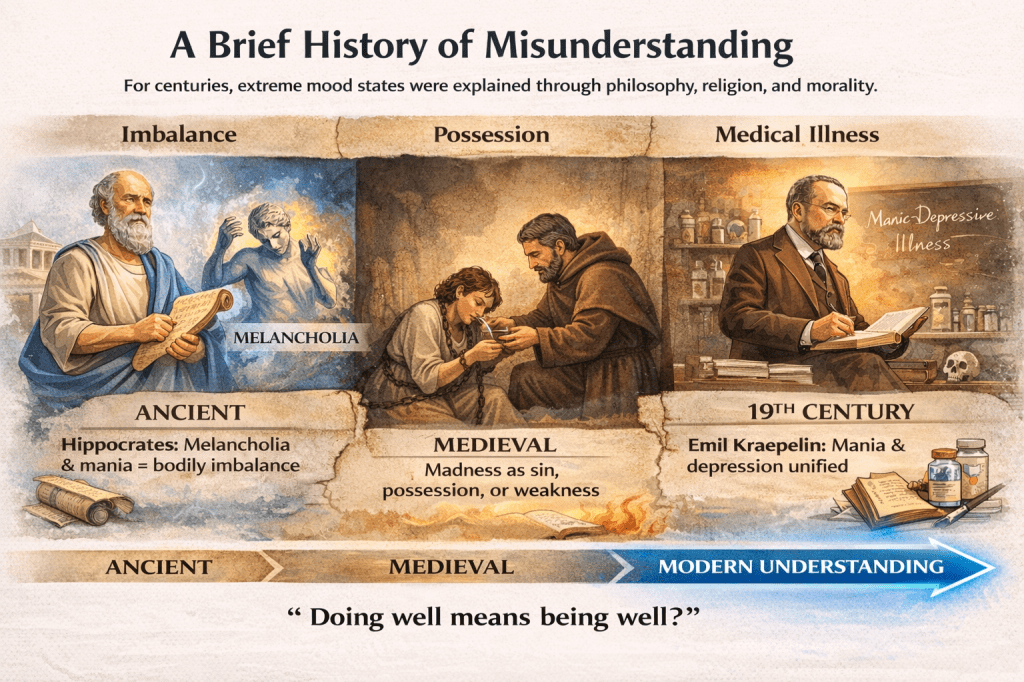
What If Our Understanding Isn’t Perfect?
Some philosophers and clinicians have questioned psychiatry’s definitions and treatments, warning against:
- over-medicalization,
- loss of meaning,
- and lack of patient voice.
These critiques matter. But even critics agree on one thing:
Severe mood crises are real, dangerous, and require care.
Questioning models should never mean ignoring risk.
When to Treat This as a Mental Health Emergency
A BPAD crisis requires urgent help when there is:
- suicidal thinking or behavior,
- psychosis,
- days without sleep,
- reckless or unsafe actions,
- inability to care for basic needs.
These are not failures — they are medical emergencies.
Final Message
Mental health crises are not always obvious. In BPAD, they are often misread as strength, personality, or success — until the cost becomes unbearable.
Understanding these patterns saves time, dignity, and lives.
If this information resonates with your experience or someone you love, reaching out for help is not giving up control. It is protecting what matters most.
Leave a comment